The testicles of a man in his 20s are known to contribute about 5-10mg of testosterone per 24-hour day and levels of total testosterone in the venous blood with that amount are observed to yield roughly 300-1200 ng/dL in the morning at the diurnal peak.
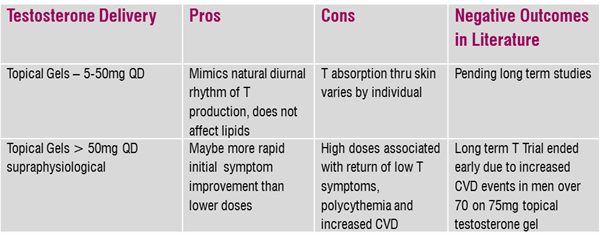
Testosterone, whether endogenous or given exogenously, negatively feeds back on the hypothalamus, limiting GnRH and thus LH and FSH from the pituitary. A man taking supraphysiological doses of testosterone can expect to have very low or undetectable levels of LH and FSH in the serum. What happens when the prescription dose overshoots the patient's optimal dose? Certainly, we see LH and FSH practically disappear.
Additionally, there can be a return of all or some of the original hypogonadal symptoms which could be due to down regulation of the tissue receptors. This is something we see demonstrated quite a bit here in the lab, especially with doses of topical testosterone gels over 50mg per day. An interesting area of research right now is androgen receptor sensitivity measured by a genetic finding (CAG repeat polymorphism), the increasing degree of which is negatively correlated to testosterone tissue uptake.
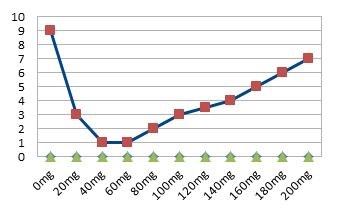
Illustration 1: Topical Testosterone Dose vs Symptom Severity VAS 1-10 in Men
What is Andropause?
Andropause can have different presentations for each individual patient. Late onset hypogonadism (LOH) is a form of secondary hypogonadism appearing in men over 40. Estimated prevalence climbs as high as 30% in men over 70 and its symptoms seem to embody the term of andropause the best. Interestingly, there’s a higher prevalence in men with type II diabetes and sleep apnea. Though there are quite a few general afflictions associated with LOH, the key symptoms are sexual and the clinical sign is low total and free testosterone in the serum. All of the above are needed for diagnosis of LOH. Psychological and physical symptoms are supportive but not diagnostic alone.
Low T – sexual symptoms
- Frequency of morning erections (<1 per month)
- Sexual thoughts (<2-3 times a month)
- Erectile function suitable for intercourse (almost never)
Low T – psychological symptoms
- Sadness
- Low energy
- Fatigue
Low T – physical symptoms
- Inability to walk more than 1 km
- Decreased flexibility – can’t bend or kneel
- Not able to engage in vigorous activity
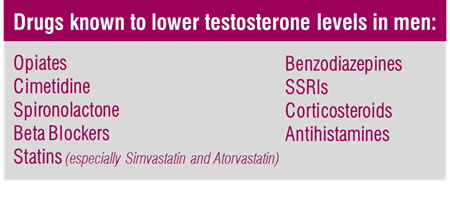
Most men with age-related low testosterone levels are asymptomatic. Clearly, there are other factors at play. Common drug therapies and nutritional deficiencies like low vitamin D levels are associated with lower levels of free testosterone. The endocrine system has intricate ins and outs, and dysfunction in one part can change the way the whole system functions. Adrenal and thyroid functions are altered by stress and changes in cortisol, T3 and T4, LH, FSH, SHBG and prolactin may be the beginning of where we see low free and total testosterone levels in a lab test turn into noticeable symptoms.
Recent studies have shown that dosing with supraphysiological amounts of topical testosterone may actually be involved in increasing the risk of cardiovascular events in elderly men rather than preventing them as seen endogenously when testosterone levels are replete.
Why are we even seeing prescribing in doses higher than normal physiological production? Larger than physiologic doses of topical testosterone are often needed in order to see total testosterone in serum studies rise and when dosing is started too high to begin with, it can be confusing to follow the symptom picture. For instance, if the starting prescription is 50mg and the patient's optimal zone (bottom of the U) is 10-20mg, even if the patient initially improves, we'll eventually see mood and sexual symptoms return. Starting at low doses and increasing them over time will help create a patient's own U-shaped curve and prevent diminishing returns.
What to check when the numbers look good but symptoms remain while on TRT:
- Estradiol levels. Testosterone becomes estradiol with the help of aromatase. This enzyme exists in nearly all body tissues including fat tissue, the gonads, blood vessels, brain and the skin. If estradiol is rising with testosterone therapy, an aromatase inhibitor may be required.
- SHBG levels. Testosterone circulates bound to SHBG at a high percentage. If SHBG is becoming elevated, free testosterone will decrease and symptoms usually appear.
- DHT levels. Testosterone metabolizes down to DHT at the tissue level via 5-alpha reductase. Elevation in DHT seems to be correlated with an increase in erythrocytosis so also assess hematocrit.
- DHEA-S levels. It could be that low androgen symptoms are attributable to low levels of this largely adrenal androgen.
- Thyroid function. Symptoms often overlap with symptoms of low testosterone.
- Diurnal free cortisol to assess for physiological stress response which may be playing a role in symptom development.
Treat the Lab or Treat the Person?
Is there a risk associated with NOT treating a low testosterone level in the asymptomatic (according to the diagnosis criteria) man? I would argue that the answer is yes. This doesn’t necessarily mean give everyone testosterone when it's low in the serum. For instance, imbalances in estradiol, free testosterone and DHEA can profoundly affect a man’s cardiovascular risk profile. After all, he is more likely to die of heart disease than any other disease. We have learned how strongly endogenous testosterone is involved in cardiovascular autonomic tone and lower T levels are associated with incidence of atrial fibrillation, type 2 diabetes, obesity, and peripheral artery disease.
Perhaps the popularization of treating menopause with hormonal therapies has encouraged men to see their own age-related decline in sex hormones as an imbalance to be corrected, but men in their 50s are seeking medical care looking for testosterone. It isn’t surprising to see that men over 40 are not okay with a hampered or discontinued sex life, low energy and mood, or muscle weakness and the eventuality of a sedentary remaining existence – a terrible lifestyle combination for cardiovascular risk.
The symptoms of low testosterone are shared with other conditions and this can be a major pitfall for patients and clinicians alike. In these cases, correcting a low serum testosterone to normal levels through testosterone prescription won't make the symptoms improve. Sorting all of this out can be a huge challenge but is often a solvable problem by digging further into the sex hormones and remembering the U-shaped curve.
