
"You have a 5-inch tumor in your chest" were the words spoken from a friend and radiologist as we both stared bewildered at my chest X-ray, following a host of side effects I'd been having for weeks.
As I looked at the X-ray film in amazement, my thoughts quickly changed to frustration and anger as I realized my behaviors and actions played a pivotal role in creating my disease—non-Hodgkin's lymphoma.
Here's the Back-story:
The year before, in my mind, I was "living the dream." I had recently received board certification in neurology, and my practice was the busiest it had ever been. The fruits of my work allowed me to purchase a new home, and sock away money for retirement. I was also involved in a relationship that was moving in the right direction, or so I thought.
Then my world began to implode. At the busiest time of my career, I discovered that a trusted employee was stealing from me (and her insurance company) in order to support a very well hidden drug habit—heroin addiction. In the midst of major renovations to my new house, my relationship turned sour. Dealing with stress both at the office and at home—day after day, week after week, month after month—became the norm.
I plugged along in the office and at home, while keeping my emotions bottled up—my usual "MO." While juggling the stressors, I ate unhealthful foods and drank red wine to help calm my nerves and sedate myself to sleep.
For the most part, that didn't work, as I lay in bed awake at night with my stomach twisting in knots as I contemplated my personal hell.
Months later, after the major crises were over, I began to feel "off." I developed a progressive fatigue as if I was fighting an infection, which caused me to struggle in the gym. At the same time I was losing weight although my appetite was back to normal and I was eating plenty.
In addition to the weight loss and fatigue, I developed throbbing headache pain when I bent over. Headaches are something I had never experienced before.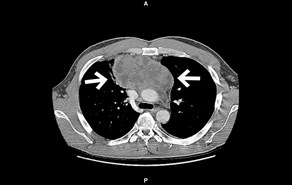
In addition to the strange and painful headaches, I developed drenching night sweats. Not like the skin sheen you get when your immune system is fighting the flu, but bed-soaking sweats. Now I knew something was seriously wrong. I rushed to the lab and had my blood drawn, to find that my level of lactate dehydrogenase (LDH)—a biomarker indicating tissue destruction—was off the charts.
These results sent me flying to the radiologist where, in one haunting moment, I was told I had a massive tumor in my chest.
We often hear stress is dangerous, but here was the disturbing proof.
What is Stress?
Stress is a momentary threat—whether perceived or physical—which creates an adaptive response in the body to ensure survival. The stressors that elicit the reaction can be physical, such as an infection, toxin, or trauma. They can also be emotional, which can include abuse, guilt, fear, loss of a loved one, or any other source from work, home, or family.
Stress and the ensuing stress response are needed to maintain survival in moments of a perceived threat, emotional or physical. Exercise is a beneficial physical stressor with its surge of hormones, vascular and muscular changes, and metabolic demands. Once stopped, the body comes back to a normal resting state.
Momentary emotional stressors also create physiological changes in response to a specific event. Under emotional stress, the brain and body release targeted hormones, along with other brain chemicals, in response to the perceived threat. These acute stress reactions and ensuing hormone release are temporary. Once the perceived threat has passed, the body should also come back to its normal state.
The stress reaction is the body’s way of preparing itself for “fight or flight.” Stress becomes a health hazard only when the stressors are constant and the physical stress response doesn't stop.
When we don’t return to our normal pre-stress set point—our normal physical and emotional state—the result is disease.
The Stress Reaction
Under stress, the hypothalamus in the brain tells the pituitary gland to secrete the hormone ACTH. ACTH travels quickly to the adrenal glands, which then secrete the hormones cortisol, adrenaline, and norepinephrine.
Adrenaline: Under stress, adrenaline causes an increased heart rate and constriction of blood vessels; it dilates your air passages and increases your energy.
Norepinephrine: Norepinephrine helps to provide energy. It increases your heart rate, as well as oxygen to the brain, and blood flow to the muscles.
Cortisol: Cortisol helps to increase blood sugar while under stress; aids in the breakdown of protein, fat and carbohydrates, which provide us with energy; and acts as an anti-inflammatory.
The stress reaction in the body is vastly complex, involving different organs, metabolic systems, and hormones. Momentary stressors cause a quick squirt of stress hormones into the bloodstream to prepare for the threat.
Typically, the physical symptoms of stress include: aches and pains, dizziness, diarrhea or constipation, chest pain, and rapid heartbeat. Emotional symptoms of stress include anxiety, moodiness, irritability, and agitation.
The Cancer Microenvironment
Cancer is a disease of altered gene expression originating with changes in the DNA. For a cell to become cancerous, it has to acquire different phenotypic behaviors that result from its genotype. Cancer development is a multi-step process caused by the accumulation of genetic errors that control cellular processes.
When a cancerous tumor has developed, its microenvironment is made up of different cell types including fibroblasts, nerve cells, endothelial cells, and infiltrating immune cells. All of these cells can produce pro-inflammatory cytokines and growth factors that support tumor growth and malignant transformation.
Cancer initiation, promotion, progression, and metastasis are intricate steps in the development of malignant tumors. These steps include genetic alteration without repair, cell growth and proliferation, evasion of apoptosis (programmed cell suicide) and the immune system, angiogenesis, and eventually metastasis from the tumor’s original site.
How Stress Affects the Cancer Microenvironment
In addition to the fuel glucose and arachidonic acid, and growth factors including insulin and 16‑hydroxyestrone, the stress hormones adrenaline, norepinephrine, and cortisol play a major role in all steps of the development and progression of cancer. A study published in Nature Reviews found that the release of stress hormones can compromise DNA repair mechanisms, leading to the development of cancer. As cancer develops into a tumor, the hormones cortisol, adrenaline, and epinephrine have a major impact on the biology of the tumor and its surrounding environment.
Often cancer evades the immune system through different mechanisms. Natural Killer (NK) cells are cytotoxic lymphocytes that rapidly respond to infectious agents and tumor formation. Their role is to seek and destroy cancer cells, as well as cells infected by viruses.
When cancer cells metastasize from their original site, they become dangerous. They invade other tissues or organs, and start the process of developing more tumors. |
Data published in Nature Reviews found that elevated cortisol suppresses the function of the NK cell, thus allowing viruses to take hold and cancer cells to survive in the body. Individuals under constant stress often have outbreaks of shingles and/or cold sores; for some, stress causes the diagnosis or return of cancer. Additional research in The Lancet found that stress-induced suppression of NK‑cell activity caused tumor development.
Suppression of NK cells increases susceptibility to infectious agents; influences the severity of infectious disease; diminishes the strength of immune responses to vaccines; reactivates latent herpes viruses; and slows the healing of wounds.
In addition to NK cells, cytotoxic T (CT) cells, another group of cancer-killing white blood cells, recognize cancer by a certain ligand (flag) on the surface of cancer cells and target them for destruction. Like NK cells, CT cells attach to the cancer cell and inject powerful enzymes into it, eventually leading the cancer cell to cause its own cell death. Cortisol, adrenaline, and norepinephrine reduce the ability of CT cells to “see” cancer cells and tumors.
All cells have a program that allows them to commit suicide when they get damaged, or cease to function normally. This programmed cell death is called apoptosis. Cancer cells also have this program. However, mutated cells have a way of escaping (evading) this self-destruct program. Researchers found that the hormones adrenaline and norepinephrine both inactivate the suicide program in cancer cells, thus allowing them to survive.
Adrenaline and norepinephrine both act in the cancer and tumor microenvironment by allowing tiny one-millimeter tumors to create their own blood supply. This process of creating new blood vessels is called angiogenesis.
Lastly, when cancer cells metastasize from their original site, they become dangerous. They invade other tissues or organs, and start the process of developing more tumors. Once the cells migrate into circulation, they can survive only if the environment favors their survival.
Beyond the Cancer Microenvironment – Effects of Stress on Cancer Spread
The majority of mutated cells die on their journey through the body, or are picked off by the immune system. A research study published in Cancer Research demonstrated that epinephrine not only suppressed the immune system when cancer cells were on the move, it removed any road blocks regarding movement and migration of cancer cells, allowing the process of metastasis to happen.
However, under prolonged stress, the hormones adrenaline and norepinephrine can increase the migration of cancer cells. In Cancer Research, evidence was presented that found norepinephrine to increase the movement and migration of colon-cancer cells. It was also found that adrenaline and norepinephrine allow cancer cells to release enzymes that dissolve the protective layer around organs, allowing the cancer cells to invade those organs.
The Role of Pro-Inflammatory Cytokines
The stress reaction is also fueled by a secondary source: cytokines and inflammation. The pro-inflammatory cytokines IL‑1, IL‑6 and TNF (tumor necrosis factor) all contribute to the development of tumors. The role of IL‑6 in cancer-cell proliferation and survival is well documented.
An article in the Journal of Clinical Investigation states that IL‑6 plays a pivotal role in the development of Kaposi’s sarcoma and multiple myeloma. IL‑6 has also been found to contribute to other cancers, such as colon cancer, lymphoma, breast cancer, and others. IL‑1 was found to increase tumor invasiveness and metastasis.
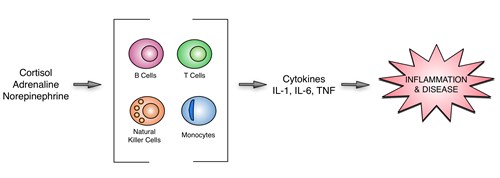
At the site of tumor development, IL‑1 caused the tumor to adhere to healthy tissue, and it assisted malignant cells in invading distant tissues. In the same research study TNF, another cytokine involved in inflammation, was shown to enhance tumor progression, stimulate angiogenesis and metastasis, and impair the immune system by suppressing the white blood cells responsible for killing cancer cells.
Summary
Stress is a serious issue, and its reaction creates a combustible fuel that creates and contributes to the progression of cancer and tumor development. From initial DNA damage and failed repair, to immune suppression, angiogenesis, and metastasis, the stress hormones cortisol, adrenaline, and norepinephrine all play a role in carcinogenesis.
Resolving chronic disease like cancer should always include helping individuals to manage their stressors. This, coupled with implementing changes in lifestyle via diet, exercise, elimination of toxins, will not only prevent the development of cancer, it will improve treatment outcomes and reduce the rate of recurrence.
Related Resources
- Blog: How to Use the Cortisol Awakening Response in Addressing Adrenal Function
- Blog: Diurnal Fluctuations in Norepinephrine & Epinephrine as Part of the Health Stress Response
- Blog: Is it Adrenal Fatigue? Reassessing the Nomenclature of HPA Axis Dysfunction.
References
- Perspectives, March 2006, Vol 6, The influence of bio-behavioural factors on tumour biology: pathways and mechanisms
- Clinical Cancer Research 2003;9:4514-4521 Stress-Related Mediators Stimulate Vascular Endothelial Growth Factor Secretion by Two Ovarian Cancer Cell Lines
- Ronald Glaser and Janice K. Kiecolt-Glaser, Stress-induced immune dysfunction: implications for health, Nature Reviews; Volume 5, March 2005; 243
- Schafer ZT, and Brugge JS. IL-6 involvement in epithelial cancers. The Journal of Clinical Investigation 117 No.12 Dec. 2007
