
The decision to start a regimen of iodine supplementation should be based on a detailed nutritional, physical, and laboratory assessment. Once the need is established, some clinicians go straight for supraphysiologic dosing while others may implement a diet rich in sea vegetables to get the job done. How do you decide where to start? The first step is understanding the different supplement forms of iodine.
Supplementation
Iodine exists in several oxidative states in the body which perform vastly different actions. That said, there are a couple of forms of iodine to understand before starting to prescribe iodine. A working knowledge of these forms is needed before diving into testing the markers of iodine status because as those markers inform the course, the form and dose will determine the outcome.
Iodide
You’ll find it in supplements typically as potassium iodide (KI). Iodine, in the form of iodide, concentrates in the thyroid gland and any other tissue with the right sodium iodine symporter (NIS) protein to bring it in – NIS concentrates iodide not only in the thyroid, but also in the cervix, the ovaries, placenta, eyes, skin, and lactating breast [1]. This is the form of iodine that gets incorporated into thyroid hormones which transport iodine around to the entire body by T4 to T3 conversion intracellularly thereby supporting a myriad of processes from basal metabolism to ovulation to the immune system. This is the form used to support the thyroid primarily along with the rest of the body. So, if you’re looking to support the thyroid and its T3 and iodine delivery service, KI may be a good choice.
Dosing range is typically 150 µg – 1100 µg (0.150 mg – 1.1 mg) daily.
I2 (Molecular Iodine)
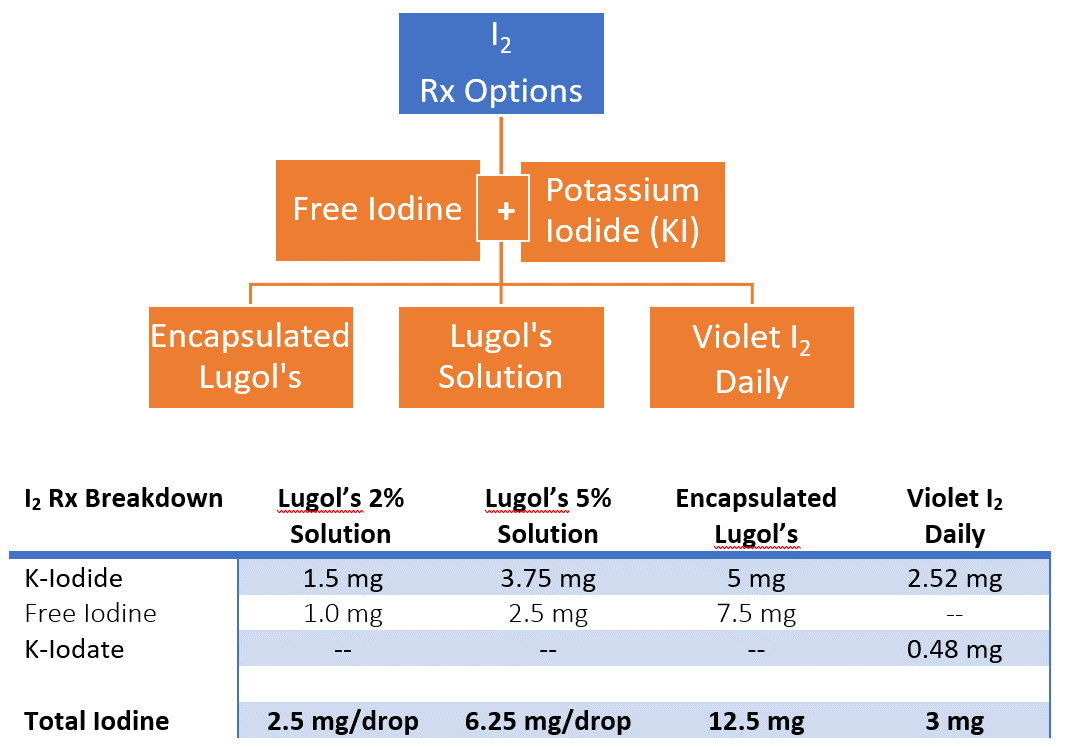
Quite different from iodide, I2 (aka molecular iodine as referred to in the literature), passes into body tissues in a NIS-independent fashion by facilitated diffusion. It lends more of an antioxidant, anti-proliferative effect to tissues by virtue of its structure and ability to form protective iodolactones and iodinated lipids - rather than concentrating in only the NIS-rich tissues as iodide would [1]. You’ll notice when you read the label of any “molecular iodine” supplement that I2 is supplemented as a mixture of potassium iodide (KI) and iodate (KIO3) or potassium iodide and free iodine. And free iodine may be referred to as elemental iodine or even molecular iodine depending on where you read about it. The mixture of KI and KIO3 forms molecular iodine (I2) “in solution” in the low pH of the stomach as it’s absorbed; the mixtures of free iodine and KI work from the premise that KI improves solubility/absorption of the free iodine portion, and transdermally-applied free iodine seems to be taken up locally as molecular iodine [2].
Once absorbed and taken up into the body, some studies show I2 doesn’t affect thyroid markers (which is good news for some patients) but does enter the breast, the prostate, tumor sites, and cystic areas, acting at the mitochondrial level to attenuate benign and cancerous growths [3]. So, this is the form to use when attempting to avoid thyroid uptake and to push the reactive oxygen species (ROS) scavenging and cell cycle-limiting effects of iodine in other parts of the body.
Dosing range is typically 1100 µg – 12,500 µg (1.1 mg – 12.5 mg) daily.
*Supraphysiologic dosing is anything over 1100 µg (1.1 mg) although a 2013 paper exploring some of the extrathyroidal actions of iodine recommended at least a 3 mg daily intake of I2 [3].
Here are some examples of such forms currently available to patients – this is in no way an exhaustive list, just an idea of what’s out there.
Caveat(s): It is possible that any of the iodine Rx options listed above will have some iodide effect on the thyroid and caution should be exercised even with the ones that claim 100% conversion to I2. Regarding iodine testing, when supraphysiologic doses of iodine are used (even transdermally), urinary iodine excretion skyrockets into the thousands. For instance, with a 12.5 mg dose, expect to see lab results between 1,000 and 3000 µg/g Cr! Higher doses yield even higher lab results even days after a dose. For sufficiency, the normal laboratory range for general thyroid health is 100 – 380 µg/g Cr.
Hashimoto’s
When anti-thyroid antibodies contribute to thyroid dysfunction, recommending iodine supplementation may feel like a dangerous undertaking. Many providers don’t recommend it at all. As a matter of fact, it’s not uncommon for ZRT to see someone with Hashimoto’s have urinary iodine labs in the severely deficient range of less than 30 µg/g Cr. That said, there are some providers treating autoimmune thyroiditis with mega-doses of molecular iodine sometimes upwards of 100 mg per day. Yes, that’s milligrams! And amazingly, these doses don’t seem to put the average patient’s thyroid into a storm (not reliably anyway) and some case reports tout complete resolution despite the inherent risk. For those of us worried about hurting the one person that does react negatively to a high dose of iodine, perhaps there’s a middle ground.
It makes good clinical sense to ensure that even our autoimmune patients receive properly monitored nutrition for their thyroids and the rest of their iodine-sensitive tissues. After all, those iodine levels can be monitored for sufficiency in the urine while other work is underway to quiet the immune system and relieve the oxidative stress of autoimmune disease [4]. It makes sense that the supplemented form be mostly molecular iodine to minimize the impact on thyroid hormones and keep the thyroid as quiet and happy as possible. And of course, using the thyroid hormone prescription to keep TSH within the normal range (NOT LOW!) ensures the NIS system will still be working hard to bring nutritionally acquired iodine into the body tissues, and any supplemented T4 will support the transport of iodine around the body where it’s needed.
Dosing range is conservative with frequent monitoring: 150 µg – 1100 µg (0.150 mg – 1.1 mg) molecular iodine with the general rule of start low, go slow. Even a low dose can cause slight changes in the thyroid hormones [5].
Final Thought on Iodine: Support and Thwart
Iodine performs some crucial roles in the body within multiple systems but it never acts alone. Depending on the environment, iodine can oxidize, reduce, and form complexes. Without stacking the deck in favor of reduction, too much iodine in the body can be destructive and may even increase the risk of autoimmune thyroiditis [6]. Once you identify low iodine status in an individual, it is absolutely imperative to assess and support iodine’s equal partners - selenium, iron, magnesium, zinc, B6, cortisol, glutathione - and consciously work to identify and thwart the endocrine disruptors like bromine, cadmium, mercury, and arsenic in order to get the best outcome [7].
Related Resources
- Webinar: Helping Patients with Hashimoto's Disease Webinar
- Handout: Iodine Deficiency - The Basics
- Blog: How to Get Enough Iodine through Your Diet
References
1 Kaczor, T. Iodine and cancer: a summary of the evidence to date. NMJ June 2014: 6(6).
2 Gottardi W. The uptake and release of molecular iodine by the skin: chemical and bactericidal evidence of residual effects caused by povidone-iodine preparations. J Hosp Infect. 1995;29(1):9-18.
3 Aceves C, et al. The extrathyronine actions of iodine as antioxidant, apoptotic, and differentiation factor in various tissues. Thyroid. 2013; 23(8): 938–946.
4 Soriguer F, et al., Iodine intakes of 100-300 μg/d do not modify thyroid function and have modest anti-inflammatory effects. Br J Nutr. 2011;105(12):1783-90.
5 Reinhardt W. Effect of small doses of iodine on thyroid function in patients with Hashimoto's thyroiditis residing in an area of mild iodine deficiency. Eur J Endocrinol. 1998;139(1):23-8.
6 Palaniappan S. Improving iodine nutritional status and increasing prevalence of autoimmune thyroiditis in children. Indian J Endocrinol Metab. 2017;21(1):85-89.
7 Chen A, et al. Thyroid hormones in relation to lead, mercury, and cadmium exposure in the National Health and Nutrition Examination Survey, 2007-2008. Environ Health Perspect. 2013;121(2):181-6.
