
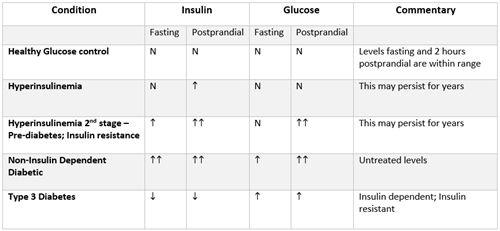
Many times when I am talking to a practitioner about a patient with PCOS and/or weight issues, I commonly get the response – "His/her blood sugar is normal." However, when we are looking at the health of PCOS and weight-challenged patients, their insulin response is of primary importance, and not just their blood sugar.
When we are fasting, both blood sugar and insulin levels should be at a steady state. Blood sugar is generally between 70-90 mg/dL and insulin levels between 1-8 µIU/mL. When we eat a meal, blood sugar increases. In response, insulin is produced by the pancreatic beta cells to help shepherd glucose into all cells to be used as energy.
Within 2 hours, insulin and glucose levels should have essentially returned to normal. Thus, our cells’ exposure to glucose and insulin is only for short blips of time within a 24 hour cycle. Excess glucose that is not used for energy is stored as glycogen in the liver and muscle cells to be used for energy between meals, where it is rapidly available for sudden energy needs such as "fight or flight" situations; but once these stores are full, the body stores extra glucose as fat in adipose cells and we gain weight.
If we allow this hyperinsulinemia to continue the body will lose the ability to manufacture enough insulin to control postprandial glucose levels. |
Insulin Resistance
When we become insulin resistant, things change. The first tissue to become insulin resistant is generally our muscle cells. Exercise improves insulin sensitivity. But when tissues become insulin resistant, higher levels of insulin are needed to shepherd glucose into cells. In a healthy situation, the pancreas responds to higher blood glucose levels by producing larger amounts of insulin to match the higher level of glucose returning glucose levels to normal with the higher insulin. Initially, this higher insulin production occurs only after meals when glucose levels spike. If, however, glucose levels after meals continue to be elevated, eventually fasting insulin levels will be elevated to maintain normal glucose levels. This situation of high insulin is called hyperinsulinemia and all of this occurs in the presence of normal blood glucose.
If we allow this hyperinsulinemia to continue, and dietary and other lifestyle choices continue to push blood sugar higher after meals, the body will lose the ability to manufacture enough insulin to control postprandial glucose levels. If insulin levels cannot control postprandial (PP) glucose levels and lifestyle continues to favor high glucose foods, fasting glucose levels will also become chronically elevated and the patient will officially have non-insulin dependent diabetes (NIDD). In a non-controlled NIDD patient, high glucose will continue to spur high insulin levels until the pancreas no longer produces adequate levels. This will stimulate an NIDD patient into an insulin deficiency state and eventually over into an insulin dependent AND insulin resistant diabetic situation, sometimes known as type 3 diabetes.
It is easy to see as we lay out the manner in which many people become diabetic, that this is not a disease that starts all at once. There are many steps along the way when we wish that patients would empower themselves to change the course of their disease.
Women with PCOS are commonly in a hyperinsulinemic state for years. It may be that they have defective insulin receptors that do not trigger adequate glucose management even at lower glucose levels. As a result, the insulin appears to drive testosterone and DHEAS higher, since the production of these hormones is stimulated by excess insulin. This higher DHEAS and testosterone from both the ovaries and adrenal glands produce so many of the symptoms of PCOS – increased facial and body hair, loss of scalp hair, and acne. The high insulin contributes to irregular menstrual cycles and drives weight gain, both by increasing food cravings, decreasing satiety, increasing adipose deposition, and changing cortisol metabolism. Women with PCOS also have altered Cortisol and HPA axis functioning. Although the mechanisms are still under investigation, many women with PCOS are found to have altered cortisol metabolism both systemically and within adipose tissues, perhaps because of their PCOS and perhaps because of obesity.
How do You Know if Someone is Hyperinsulinemic?
Symptoms of hyperinsulinemia include fatigue which may be severe, complaints of "hypoglycemia" even in the presence of normal or high-normal glucose levels, weight gain, acne, increased facial/body hair, loss of scalp hair, browning of the skin in areas of rubbing (neck and armpits are common – known as acanthosis nigrans), skin tags, anxiety, depression, brain fog, sugar cravings, and a sensation of never being full.
So the next time you see that PCOS patient or overweight patient who tells you that they are not diabetic consider that hyperinsulinemia might still be contributing to a lot of their symptoms.
