
Neurotransmitters 101
The brain orchestrates the delicate interplay between the body and the mind. Structural brain units, the neurons, discharge neurotransmitters. These neurotransmitters provide a communication platform for the brain to fuel internal systems with information.
Anything the body senses, feels, hears, smells, touches, or ingests serves as an input that prompts an astoundingly fast response. In the central and peripheral nervous system, neurotransmitters operate as chemical messengers that relay the signal and receive feedback via electrochemical impulses to regulate cognition, memory, emotions, respiration, heart rate and contractility, digestion, metabolism, blood flow and pressure, and hormonal responses. When released from peripheral organs, neurotransmitters can also behave as hormones by diffusing to distant sites via the circulation.
Etiology of Suboptimal Psychological Well-Being
The etiology of mood disorders is profoundly complex and likely encompasses many different types of neurotransmitters, how they achieve balance in the brain, and how they each interplay with other hormone systems throughout the body. Appropriate balancing of neurotransmitter signals allows the body to maintain equilibrium. When brain and peripheral neurochemistry become unbalanced, the body will struggle to re-establish physiological integrity, which may present in the form of suboptimal psychological well-being. Excessive or deficient levels of certain neurotransmitters in both the brain and in the periphery are associated with a spectrum of neurobiological disorders, such as depression and anxiety.
An Epidemic of Mood Disorders
Millions of people in the U.S. suffer from mental health disorders – mood disorders are the third most common cause of hospitalization in the U.S. for individuals aged 18 to 44. Nearly 7% of American adults live with major depression and approximately 18% live with anxiety disorders such as panic disorder, obsessive compulsive disorder, posttraumatic stress disorder, generalized anxiety disorder, and phobias [2]. Not surprisingly, the top-prescribed and top-selling prescription drugs in the U.S. in 2014 included antipsychotics, antidepressants, and attention-deficit disorder drugs [3].
Current Treatment Paradigm Lacks Specificity
The current treatment paradigm in addressing suboptimal brain health relies on diagnostic approaches that encompass the evaluation of clinical signs and adverse symptoms. Despite the lack of testable biomarkers for mood disorders, for many patients treatments can generally be effective. However, profound variability in individual response to treatment may hamper progress towards satisfactory outcomes (Fig. 1). And even after treatment frequent relapse episodes can still happen. Furthermore, a large number of patients suffer from treatment-resistant depression [4]. Therefore, selection of the best therapeutic regimen for each patient remains a tremendous challenge, and is often discovered through a time-consuming process of trial and error. Also, no single approach works for everyone with any one disorder.
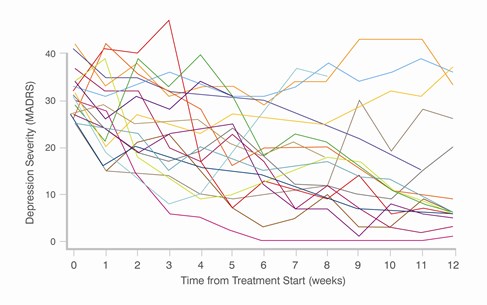 Fig. 1 Vast individual variability response to treatment of depression (adapted from [1])
Fig. 1 Vast individual variability response to treatment of depression (adapted from [1])
How to Achieve a Diagnostic Edge When Treating Mood Disorders
Targeted neurotransmitter testing can help health care practitioners achieve a diagnostic edge beyond the traditional psychological inventory. Specific biochemical heterogeneities for each particular patient can be identified based on neurotransmitter test results, thus allowing practitioners to objectively monitor therapeutic responses during and after intervention. Neurotransmitter testing enhances medical assessment and represents a major advance in the personalization of the treatment of mood disorders. The measurement of specific imbalances may be a very effective neurobiological tool in guiding targeted intervention, aimed at addressing the individual excess or deficiency in question.
Clinical Validity of Neurotransmitter Testing
The importance of effectively assessing and treating mood disorders cannot be overstated. Objectivity is a key element to the therapeutic approach to mood disorders. Currently, the standard of care dictates a trial and error pharmaceutical approach is taken with each patient based on both self and clinician assessments. However, without information yielded from objective clinical testing, selection of the most effective treatment for each particular patient with a mood disorder continues to be a challenge.
While this may prove effective for some patients, the potential for harm during those interim treatment failures is a real concern for clinicians and patients alike. Urinary neurotransmitter analysis has a breadth of data to support the efficacy of the test in clinical practice. Evaluation of neurotransmitter levels in urine provides valuable information about the heterogeneity of patient biochemistry, epigenetics, and how the body functions as a whole.
Neurotransmitter testing gives practitioners a diagnostic edge over the traditional psychological inventory. |
A common misconception is that urinary neurotransmitter measurements cannot be used to assess individual neurochemical imbalances. The degree of significance of neurotransmitter activity in the periphery is sometimes overlooked. In addition to executing vital roles in the brain, neurotransmitters are biosynthesized in the periphery to regulate essential biological processes.
Urinary neurotransmitter evaluation provides information regarding the state of a physiological condition, the function of enzymes involved in neurotransmitter biosynthesis and breakdown, and allows monitoring of the progress of therapeutic interventions. Therefore, in reality, the test provides a means to glean a functional systemic perspective regarding each neurotransmitter.
How do Neurotransmitters End Up in Urine?
Some neurotransmitters are produced in the brain and transported across the blood-brain barrier into blood, and others are produced in the periphery (e.g., norepinephrine and epinephrine). Nephrons, the functional units of the kidney, filter circulating neurotransmitters or their precursors from the blood into urine [5]. For some neurotransmitters, urinary measurements correlate with levels in the central nervous system (e.g., glutamate, PEA), and for others, what ends up in urine is only reflective of peripheral biosynthesis (e.g., serotonin, dopamine).
Regardless of production origin, neurotransmitter excretion reflects the overall systemic neurotransmitter tone, dysregulation of which may contribute to disease states. The ability to identify abnormality across specific areas of the catecholamine and PEA, GABA/glutamate, serotonin, histamine, and glycine pathways allows healthcare providers to develop a treatment plan tailored to the specific areas associated with imbalance.
Neurotransmitter Testing At ZRT
The nature of urine collection is non-invasive and preferable over the traditional invasive collection approaches such as measurement of cerebrospinal fluid. Even with liquid urine collection the patient experiences the enormous hassle of collecting all urine voids over a 24 hr period into a large jug. To circumvent this inconvenience some labs have settled for collecting only the 2nd void, limiting neurotransmitter results to a single morning time point snapshot.
ZRT Laboratory offers an alternative to the liquid urine collection method by offering a simple and convenient collection of four separate urine samples at specific time points throughout the day – 1st morning, 2nd morning (approximately 2 hours after the first collection), early evening, and bedtime. Urine is collected onto filter strips by urinating directly on the strip, or by dipping the filter card in a cup containing the collected urine. The dried urine cards are then sent to ZRT for testing. The convenience of the collection method warrants patient compliance and ease of incorporation into clinical practice.
Learn more about Neurotransmitter Testing
- Blog: Diurnal Fluctuations in Norepinephrine & Epinephrine Levels as Part of the Healthy Stress Response
- Blog: A Dynamic Duo - When to Test Neurotransmitters with Sex Hormones
- Web: Neurotransmitter Testing
References
[1] Uher R: Genes, environment, and individual differences in responding to treatment for depression. Harv Rev Psychiatry 2011;19:109-124.
[2] National Alliance on Mental Illness: Mental Illness. Facts and Numbers.; 2013.
[3] Brooks M: Top 100 Most Prescribed, Top-Selling Drugs; 2014.
[4] Eby GA, III, Eby KL: Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses 2010;74:649-660.
[5] Pestana M, Jardim H, Correia F, Vieira-Coelho MA, Soares-da-Silva P: Renal dopaminergic mechanisms in renal parenchymal diseases and hypertension. Nephrol Dial Transplant 2001;16 Suppl 1:53-59.
